Post-Thrombotic Syndrome (PTS) is a condition characterized by continuous symptoms of a blood clot, also known as deep vein thrombosis (DVT), in the leg. It causes redness, swelling, ulceration, and chronic limb pain in over a third of individuals with DVT. PTS can impair mobility and incur high treatment costs, making prevention essential. DVT primarily affects the legs.
Why is Post Thrombotic Syndrome a problem?
PTS can lead to leg ulcers and persistent leg soreness that may last for years or a lifetime. It can hinder activities like walking and standing, and treating PTS and its ulcers can be time-consuming and expensive.
PTS affects 20-40% of individuals following a lower extremity DVT episode, making it a common consequence. Severe PTS, which can result in leg ulcers, occurs in one out of every ten patients.
Factors that increase the risk of acquiring PTS:
- Being over 65 and having a blood clot in the deep veins above the knee (proximal DVT)
- Having two or more blood clots in the same leg
- Experiencing blood clot symptoms one month after initial diagnosis
- Being significantly overweight
- Struggling to maintain steady blood thinner levels during the first three months of treatment
Can PTS occur soon after a blood clot?
The onset of PTS can vary, typically ranging from six months to two years after the formation of a blood clot in the leg.
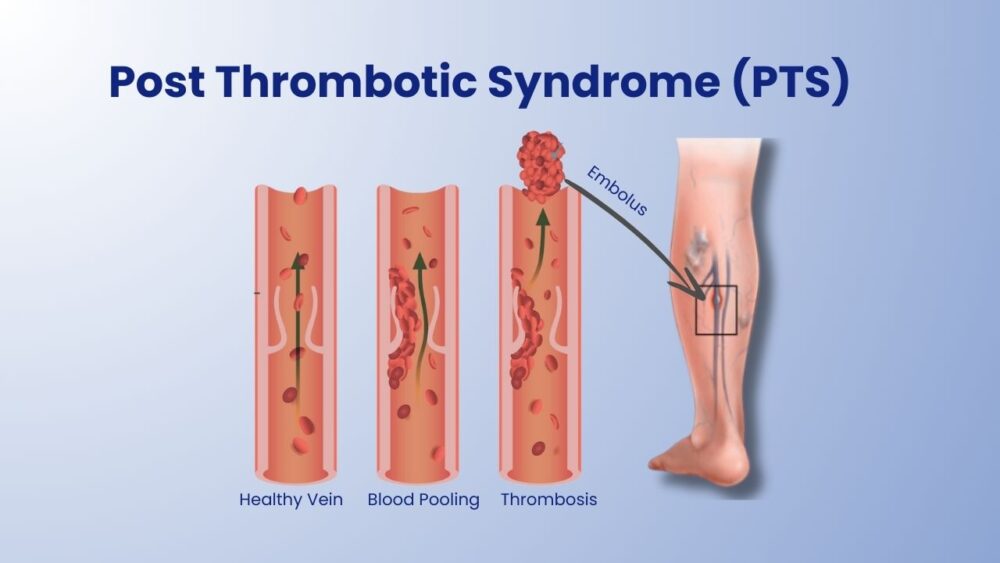
Mechanism of developing symptoms (including ulcers) in PTS
Early diagnosis and treatment of DVT are crucial to prevent severe damage. Once the vein valves and walls are damaged, they cannot be restored.
Vein valves ensure proper blood flow toward the heart but are delicate and easily damaged. When valves are compromised, blood can flow in the wrong direction, causing reflux, swelling, and discomfort in the lower leg veins.
With a DVT, the vein walls may become scarred and damaged. Increased blood flow during physical activities, such as walking, can result in throbbing pain and swelling in the lower legs. This can lead to skin dryness, discoloration, itchiness, and eventually the development of non-healing sores known as venous ulcers.
In severe cases, the vein may become completely obstructed, preventing any blood flow. This represents the most severe form of PTS.
How can I check if I have PTS?
The following are common signs and symptoms of PTS in the leg caused by a blood clot:
- Swelling that worsens after prolonged walking or standing but improves with rest or leg elevation
- Cramping
- Itching
- Tingling
- Aching or heaviness in the leg or foot
- Dry, flaky, or red skin
- Bluish or brownish pigmentation in the leg or foot
- Leg ulcers
The presence and intensity of these issues may vary from person to person. Some may experience all symptoms while others may have only a few. These sensations can be constant or intermittent.
Does having varicose veins increase the chances of getting PTS?
Varicose veins are superficial veins beneath the skin's surface and can develop due to various reasons, even without a prior blood clot. PTS, however, is caused by blood clots in the deep vein valves. If you have had a blood clot in your leg, you may develop varicose veins. A healthcare physician will examine for varicose veins to assess whether you have PTS.
Blood clots can form in varicose veins and potentially travel to the deep venous system, causing deep vein thrombosis (DVT). DVT is a risk factor for developing PTS, so it is important to consider treating varicose veins or consulting a vein expert.
What can I do to prevent Post Thrombotic Syndrome?
While PTS may be a long-term issue, prevention is crucial. Here are some steps to help avoid PTS:
Prevent blood clots from forming, as they are responsible for damaging leg veins and causing Post Thrombotic Syndrome.
Certain individuals, especially hospitalized patients or those who have undergone surgery or are bedridden, have a higher risk of blood clots. Compression boots, stockings, or medication may be provided during hospitalization and upon discharge to prevent blood clots. If you're in the hospital and haven't received these measures, consult your doctor about blood clot prevention.
If you have previously experienced a blood clot in your leg, you are at a higher risk of developing another.
To prevent a second clot, follow your doctor's instructions and adhere to the prescribed blood thinner medication, scheduling regular blood tests as directed.
Do not discontinue blood thinner medication unless instructed by your doctor. Consider treating varicose veins.
Treatment and pain management for Post Thrombotic Syndrome
Elevate your legs properly to alleviate discomfort and edema associated with PTS.
Your doctor may prescribe graduated compression stockings or a leg device to enhance blood flow, reduce swelling, and alleviate pain.
Post Thrombotic Syndrome is a chronic condition that is challenging to diagnose and treat. It often causes pain and can progress to more severe problems.
Since there is no cure for PTS, early diagnosis and treatment of DVT are essential. The faster a clot dissolves, the less damage it inflicts on vein valves and walls. Compression stockings can be used as a prophylactic measure in high-risk DVT settings like hospital stays or long-haul flights.
To learn more, visit Melbourne Varicose Vein Clinic, a highly rated clinic in Melbourne. Dr. Yazdani, a compassionate and experienced medical practitioner of over 18 years, can provide valuable insights. Book your appointment online or call us to schedule your visit.