Venous Ulcers
- Home
- Venous Ulcers
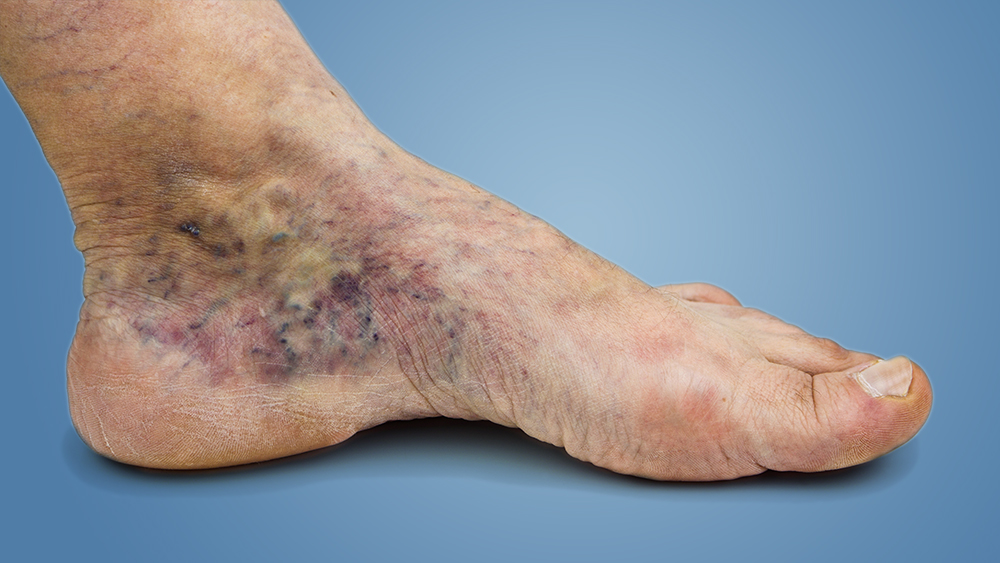
Inflammatory processes that result in leukocyte activation, endothelial injury, platelet aggregation, and intracellular edema are all possible causes of venous ulcers. Older age, obesity, prior leg injuries, deep venous thrombosis, and phlebitis are the key risk factors for venous ulcer formation. Venous ulcers are usually irregular, shallow, and found over bony prominences on physical inspection.
The ulcer base typically contains granulation tissue and fibrin. Lower extremity varicosities, edema, venous dermatitis, and lipodermatosclerosis are all common findings. Venous ulcers are often chronic and an open ulcer can last anywhere from a few weeks to several years.
Ulcers occur because of damage to the valves inside the leg veins.
Cellulitis, Osteomyelitis, and Malignant shift are all serious complications. Large ulcers’ size and lengthier healing time are also poor prognostic factors. Leg elevation, Compression therapy, Dressings, treating underlying abnormal veins can improve and expedite the healing process.
Up to 4% of people suffering from chronic venous insufficiency suffer from ulcers. Ulcer can be single or multiple, can be small or large. Venous Ulcer is usually a chronic ulcer. Ulcer management can be complex and it is crucial to be treated by an experienced phlebologist or health professional. It usually requires combined techniques. Surgical management may be considered for ulcers that are large in size of prolonged duration or refractory to conservative measures.
Read success story on Chronic Ulcer treatment
Stasis dermatitis, which causes scaling and erythema of the lower extremities, can develop as a venous ulcer develops. Hemosiderin staining, which results in brownish or yellow spots under the skin, is also possible. As a result of blood leaching into the surrounding tissue, other skin changes can include the appearance of dark red or purple.
Call Dr. Nellie to understand the stage of Ulcer in your leg. Venous ulcers usually manifest as shallow but large wounds with irregular margins on the lower leg or ankle. When manipulated, the ulcer's base is usually red, produces a large amount of exudate depending on the degree of infection, and oozes venous blood.
Older age, obesity, previous leg injuries, deep venous thrombosis, and phlebitis can be the risk factors to develop Ulcers.
In most cases, the wound would be relatively painless, with some discomfort arising from infection or edema. Stasis dermatitis causes the entire leg to swell and the skin to become hard and reddish-brown in color. Elevating the affected limb will help to alleviate pain and swelling.
Laser Ablation, Ultrasound Guided Foam Sclerotherapy, and Compression stockings could improve the healing process.
Don’t let the vein conditions get worse, step in Melbourne Vein Clinic for treatment.
Dr. Yazdani has achieved great results in solving the Vein issues.
Call Us to visit the Dr. at your convenience or Book an appointment online.
